X-rays impacts in interventional cathlabs
I – RISKS
Interventional cardiologists have the highest annual exposure to X-rays[1]. The use of X-rays during catheterisation procedures is of particular concern, especially during prolonged exposures. Many measures are taken to reduce patient exposure, but what about the operators?
Patient safety is often prioritised over operator safety, which deserves just as much attention. Today, you can save the lives of others without putting your own life at risk!
Whereas the patient is exposed to X-rays only during a limited timeframe, the medical staff deals with ionizing radiation on a consistent, repetitive basis. Each operator performs up to several hundred or even thousand of procedures per year, and the cumulative dose has to be taken into serious consideration.
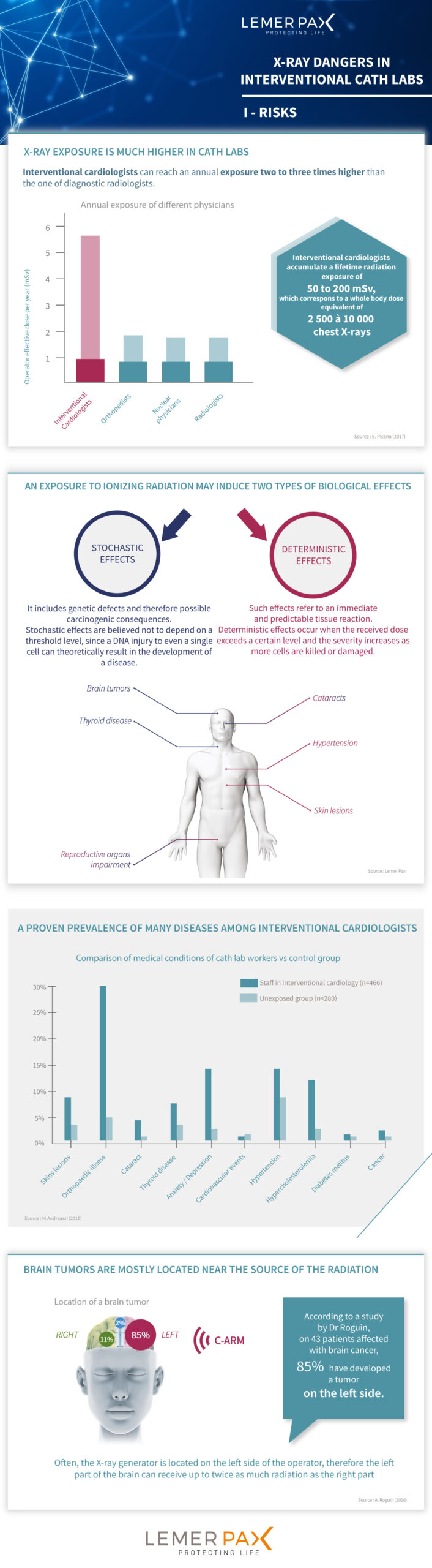
Cardiologists in most high-volume cath labs can reach an annual exposure of more than 5 mSv1: a value two to three times higher than the one of diagnostic radiologists.
AN EXPOSURE TO IONIZING RADIATION MAY INDUCE TWO TYPES OF BIOLOGICAL EFFECTS:
- Stochastic effects
It includes genetic defects and therefore possible carcinogenic consequences. Stochastic effects are believed not to depend on a threshold level, since a DNA injury to even a single cell can theoretically result in the development of a disease. Among stochastic effects are for example radiation-induced cancer and thyroid disease
- Deterministic effects
Such effects refer to an immediate and predictable tissue reaction. Deterministic effects occur when the received dose exceeds a certain level and the severity increases as more cells are killed or damaged. The development of radiation-induced skin lesions is an example of deterministic events[2].
A HIGH PREVALENCE OF MANY DISEASES AMONG INTERVENTIONAL CARDIOLOGISTS
A recent study[3] comparing medical conditions of staff exposed to X-rays versus non-exposed personnel revealed that the first group had developed higher rates of several health problems. Statistical difference was found in the development of skin lesions, orthopaedic illness, cataracts, thyroid disease, confirming previous results.
New findings of this study were discovered regarding the prevalence of hypertension and hypercholesterolemia. Anxiety and depression occurred in 12% of exposed subjects, compared with 2% of controls.
Authors suggest that this might be a newly discovered effect of radiation, which is especially relevant on the unprotected head of the operator. At chronic low doses ionizing radiation may impact detrimentally on hippocampal neurogenesis and neuronal plasticity.
BRAIN TUMOURS MOSTLY LOCATED ON THE SIDE OF THE X-RAYS SOURCE
The possible neurological impact of X-rays was suggested in 1975 by Matanoski[4]. Then, in 1998 two Canadian interventional cardiologists were diagnosed with brain tumors[5]. However, it is only in 2013, after the publication of A. Roguin[6], that awareness on this issue was raised.
In his article, A. Roguin studied a cohort of 31 interventional physicians who developed a brain cancer. More precisely, the tumors were glioblastoma multiforme, astrocytoma and meningioma.
The results showed that in 85% of cases, the malignancy was left-sided. The majority of physicians died shortly after diagnosis.
Dr. Roguin’s findings have been recently extended to an analysis of 12 additional cases, resulting in total of 43 cases of physicians exposed to X-rays[7]. In this study, data for 35 patients was available concerning the localization of the brain tumor. These results confirm that the malignancy is prevalently located on the left side. Often, the X-ray generator is located on the left side of the operator, therefore the left part of the brain can receive up to twice as much radiation as the right part[8]. This strong association suggests that left-sided brain tumors correlate with the ionizing radiation to which medical workers are exposed.
It should be noted that given the small population study, this data provides only a basis for a speculation of a direct correlation between radiation exposure and brain tumor incidence.
TO FIND OUT MORE, DOWNLOAD OUR WHITE PAPER
[1] Picano E., et al., The Radiation Issue in Cardiology: the time for action is now. Cardiovasc Ultrasound 2011 Nov 21, 9:35.
2 Sun Z. et al., Radiation-Induced Noncancer Risks in Interventional Cardiology : Optimisation of Procedures and Staff and Patient Dose Reduction. BioMed Res Int, 2013.
[3] Andreassi MG, et al., Occupational health risks in cardiac catheterization laboratory workers. Circ Cardiovasc Interv. 2016 Apr;9(4).
[4] Matanoski GM, et al. The current mortality rates of radiologists and other physician specialists: specific causes of death. Am J Epidemiol. 1975;101(3):199-210.
[5] Finkelstein MM, et al., Is brain cancer an occupational disease of cardiologists? Can J Cardiol 1998;14:1385-8.
[6] Roguin A. et al., Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol, 2013 May 1;111(9):1368-72.
[7] Roguin A., Radiation and your Brain: possible measures to reduce radiation in your cath lab. Endovascular Today Vol. 15, No. 8 August 2016.
[8] Picano E. et al., Cancer and non-cancer brain and eye effects of chronic low-dose ionizing radiation exposure BMC Cancer 2012, 12:157.