How to protect your Nuclear Medicine and Radiopharmacy department?
Nuclear medicine plays an essential role in the diagnosis and treatment of many diseases. However, the use of radioactive substances requires rigorous protection to ensure the safety of both patients and medical staff.
In this article, we explore the various aspects of radiation protection in nuclear medicine and radiopharmacy, from the risks involved to specialist equipment and the regulations in force.
Dangers and risks of ionising radiation
Nuclear medicine uses radiopharmaceuticals, which are administered to patients for diagnostic or therapeutic purposes. These medicines contain substances that emit ionising radiation.
In diagnostic procedures, they are used to obtain precise images of the functioning and/or location of an organ or tissue, or in therapeutic procedures to treat a pathology precisely. However, this radiation poses health risks if it is not properly controlled.
The main risks in Nuclear Medicine and Radiopharmacy are:
- Internal or external contamination: ingestion or direct contact with radioactive substances
- Irradiation: external exposure to ionising radiation
It is important to note that health professionals are generally more exposed than patients, due to their regular contact with radioactive sources. The effects of exposure to radiation can appear in the short term (skin lesions, cataracts, etc.) or in the long term (increased risk of cancer, etc.). This is why it is essential to have the right radiation protection equipment for your Nuclear Medicine and Radiopharmacy department.

Strict regulations
Faced with these risks, nuclear medicine and radiopharmacy are subject to strict regulations, which vary from country to country. In France, the body that regulates the use of radioactive substances in the medical field is the Autorité de Sûreté Nucléaire et de Radioprotection (ASNR), formed from the merger of IRSN, the French nuclear safety expert, and ASN, from 1 January 2025.
At international level, a number of organisations issue standards and recommendations on radiation protection:
- The International Atomic Energy Agency (IAEA) provides global guidelines for nuclear safety.
- The International Organisation for Standardisation (ISO) proposes specific standards for radiation protection equipment and procedures
- The American National Standards Institute (ANSI) establishes standards recognised in the United States and beyond
These regulations impose strict requirements in terms of equipment, staff training and safety procedures. Continuous training and scrupulous compliance with radiation protection protocols are essential to maintaining a high level of safety in health establishments with a Nuclear Medicine and Radiopharmacy department.
Precautionary principles in nuclear medicine
Radiation protection in nuclear medicine is based on three fundamental principles:


- Justification: any use of ionising radiation must be justified by the expected benefits in relation to the risks involved.
- Optimisation: radiation doses must be kept as low as reasonably achievable. This is the ALARA (As Low As Reasonably Achievable) principle.
- Limitation: doses received by individuals must not exceed regulatory limits.
The ALARA* principle is the golden rule of radiation protection. It applies to all medical structures that use ionising radiation, from nuclear medicine to interventional medicine. This principle guides the choice of equipment and procedures to minimise exposure to radiation.
*ALARA: As Low As Reasonably Achievable is one of the basic principles of protection against ionising radiation.
Radiation protection equipment
To ensure effective protection in nuclear medicine, it is essential to have the right equipment at every stage of the process, from the reception of the radionuclide on the premises, to the preparation of radiopharmaceuticals, administration and storage, right through to the management of liquid or solid radioactive waste.
Premises equipment
Staff in medical imaging departments or radiotherapy rooms are protected by:
- Shielded glass: for observing procedures while remaining protected
- Shielded furniture: for the storage and containment of radioactive sources of all energies
- Shielded doors: for biological protection of access to radiotherapy bunkers
- Shielded screens and pass-through: to secure the transfer of radiopharmaceutical doses

Radiopharmaceutical preparation equipment
The safe preparation of radiopharmaceuticals requires specialised equipment:
- Dose calibrators: for precise measurement of radiopharmaceutical activity
- Shielded preparation hot cells: for handling radioelements, for example during radiolabelling, fractionation and dispensing of radioactive substances, in complete safety.
- Preparation accessories: vial protectors, water baths, shielded stirrers, etc.
- Radiation screen shields: to protect personnel during cell labelling or quality control, etc.
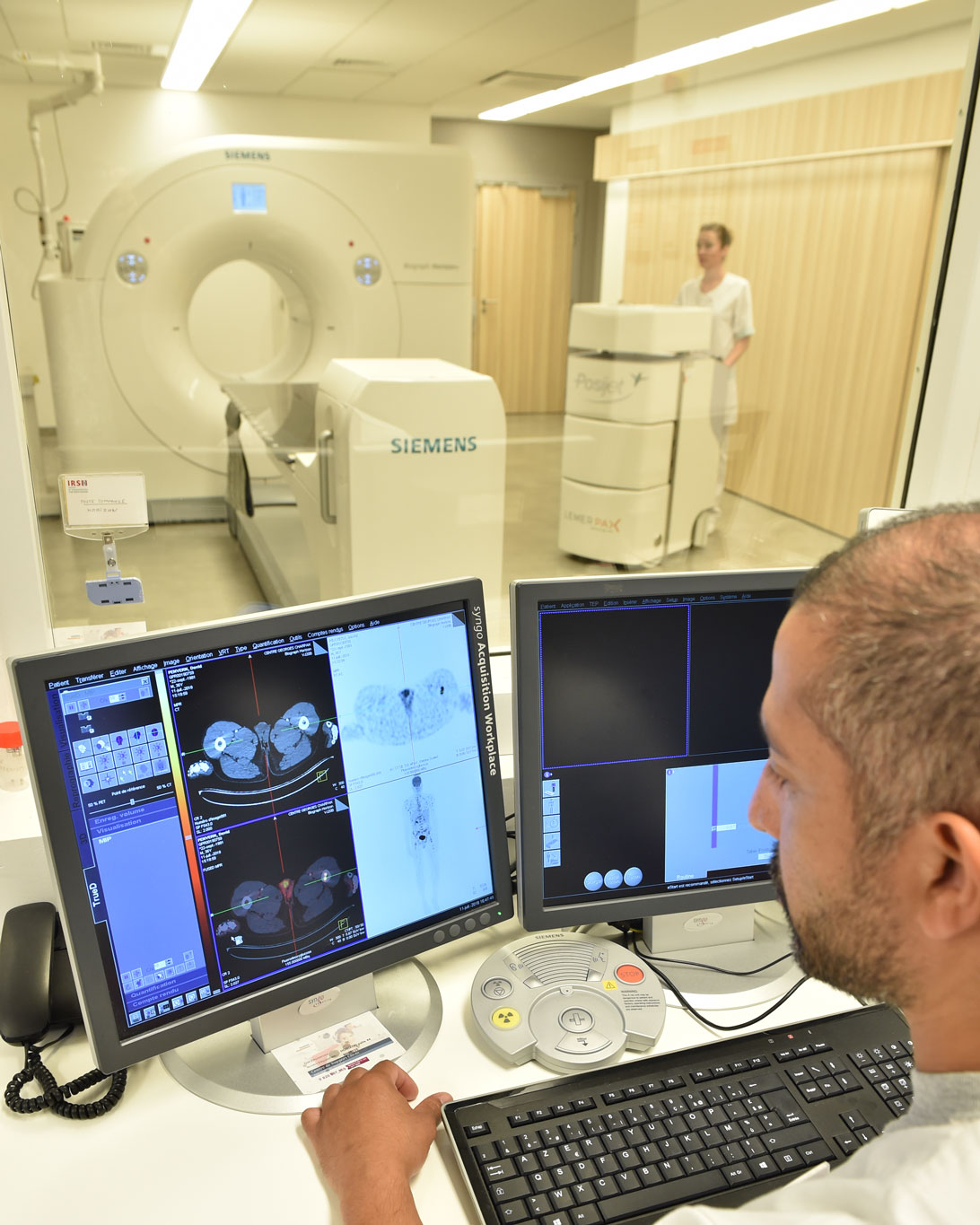
Radiopharmaceuticals administration equipment
Safe handling of radiopharmaceuticals requires specialised equipment to minimise staff exposure during patient dose preparation and administration:
- Syringe shields: for safe handling of syringes containing radioactive substances during manual injection
- Shielded carrier cases: for transporting patient syringes
- Injection shields: for extra protection during direct or indirect administration to the patient
- Shielded trolleys: for safe transport of prepared doses to the patient
- Mobile fractionation, dispensing and injection units: such as the Posijet® from Lemer Pax, which enables radiopharmaceuticals to be administered precisely and remotely, significantly reducing staff exposure.
- Shielded injection systems: for treatments requiring administration over a prolonged period, such as TheranojetARA®, designed for the safe administration of therapeutic radiopharmaceuticals, particularly in RadioPharmaceutical Therapy.


Radioactive waste and effluent storage and management equipments
The safe management of radioactive waste is crucial:
- Shielded bins: for the temporary storage of radioactive waste
- Shielded safes: for storing radioactive sources
- Separating toilets: for the safe disposal of patients’ radioactive waste
- Decay tanks: for storing liquid effluents until their radioactivity reaches an acceptable level before release
- Septic tank: for separating solid and liquid matter and partial biological degradation, thus providing primary purification
Radiation protection in nuclear medicine and radiopharmacy: innovating for the future
In a Nuclear Medicine and Radiopharmacy department, radiation protection is a complex issue that requires a global approach. It is based on:
- A thorough understanding of the risks associated with ionising radiation
- Scrupulous compliance with current regulations
- Applying the principles of radiation protection, in particular the ALARA principle
- Use of appropriate, high-performance protective equipment
- Ongoing staff training and strict compliance with safety protocols

The constant development of technologies in nuclear medicine and radiopharmacy is accompanied by innovations in the field of radiation protection. Improved materials, such as Lemer Pax’s Novashield®, offer increased lead-free protection compared with the lead found in radiation protection equipment. Automated administration systems, such as Posijet®, considerably reduce staff exposure when handling radiopharmaceuticals.
Protecting a Nuclear Medicine and Radiopharmacy department is an ongoing challenge that requires vigilance, expertise and investment in high-quality, innovative equipment. This is the only way that this essential medical discipline can continue to develop, for the benefit of patients and the safety of all healthcare professionals.
Glossary
- Radiopharmaceutical: medicine containing a radioactive element used in nuclear medicine for diagnosis or treatment.
- Ionising radiation: type of energy released by atoms in the form of electromagnetic waves (gamma or X-rays) or particles (neutrons, beta or alpha particles).
- ALARA: As Low As Reasonably Achievable, a principle aimed at minimising exposure to radiation.
- Theranostics: approach combining diagnosis and therapy, used in Nuclear Medicine.
- Cyclotron: particle accelerator used to produce radioisotopes.
- Radioactive effluents: potentially radioactive liquid waste generated by Nuclear Medicine activities.